Presentation

Our team’s research focuses on neuroblastoma, a pediatric cancer arising in the peripheral sympathetic nervous system, a tissue derived from neural crest cells. This aggressive solid tumor accounts for 15% of childhood cancer-related deaths, with long-term survival rates for high-risk cases remaining below 40%. Our primary goal is to deepen our understanding of the biology and oncogenic mechanisms underlying neuroblastoma, enabling the development of novel therapeutic strategies to improve outcomes for children with severe forms of the disease.
A major milestone in neuroblastoma research was the identification of activating mutations in the ALK gene in a subset of sporadic and familial cases (Janoueix-Lerosey et al., Nature, 2008) (Figure 1). This discovery represented a significant breakthrough in understanding the molecular basis of the disease and paved the way for the development of targeted therapies, offering new hope for affected patients.

Figure 1: Mutations of the ALK receptor tyrosine kinase in neuroblastoma. The two mutation hotspots in the sporadic forms correspond to residues F1174 and R1275. TM: transmembrane domain, TK: tyrosine kinase domain. Adapted from « Le gène ALK (anaplastic lymphoma kinase), un nouvel acteur majeur du neuroblastome ». Isabelle Janoueix-Lerosey, Olivier Delattre. Médecine/Sciences n° 4, vol. 25, avril 2009.
The ALK gene encodes a tyrosine kinase receptor predominantly expressed in the central and peripheral nervous systems. To investigate the role of ALK mutations in neuroblastoma oncogenesis, we developed genetically modified mouse models harboring the F1178L and R1279Q Alk mutations, which correspond to the F1174L and R1275Q mutations observed in patients, respectively. These models revealed that the mutations disrupt the development of the sympathetic nervous system (Cazes et al., Oncotarget, 2014). Knock-In (KI) animals exhibited enlarged superior cervical and stellate ganglia, starting from the E12.5 embryonic stage and persisting into adulthood. Transcriptomic analysis of these ganglia showed increased proliferation of sympathetic neurons at birth in the mutants, shedding light on how germline ALK mutations contribute to neuroblastoma predisposition. However, these Alk mutations alone were insufficient to induce tumor formation in mice. To assess their oncogenic potential, we crossed the KI Alk lines with TH-MYCN transgenic mice, which overexpress the MYCN oncogene under the control of the tyrosine hydroxylase promoter. These TH-MYCN mice develop neuroblastomas that closely mimic those seen in children, albeit with incomplete penetrance and a latency of several weeks. Our findings demonstrated a strong oncogenic cooperation between Alk mutations and MYCN overexpression. Notably, the F1178L mutation exhibited stronger oncogenic potential than the R1279Q mutation.
Genetic alterations alone cannot fully explain the complexity of neuroblastoma biology. To gain deeper insights into high-risk forms, we investigated the epigenetic landscape and transcriptomic profiles of neuroblastoma cell lines and neural crest cells. This work identified two distinct cellular identities in neuroblastoma, termed noradrenergic (NOR) and NCC-like/mesenchymal (MES) (Boeva et al., Nature Genetics, 2017) (Figure 2a). These identities exhibit marked differences in their behavior, including different levels of chemotherapy resistance and migration capabilities in vitro.
Further analysis revealed the transcription factor network driving the NOR identity, which includes PHOX2B, HAND2, and GATA3 (Figure 2b). These transcription factors are critical regulators of the noradrenergic sympathetic neuron specification during normal development, underscoring the parallel between neuroblastoma and its cell of origin.

Figure 2: (a) Characterization of noradrenergic and mesenchymal identities in neuroblastoma cell lines by analysis of Super-Enhancers revealed by ChIP-seq of the H3K27ac mark. hNCC: human Neural Crest Cells. (b) Network of transcription factors associated with the noradrenergic identity. Publication: Boeva et al., Nature Genetics, 2017.
In several neuroblastoma cellular models, we have documented spontaneous and reversible plasticity between noradrenergic (NOR) and mesenchymal (MES) identities, driven by epigenetic reprogramming (Thirant et al., Nature Communications, 2023). Our findings show that both intrinsic factors and microenvironmental signals play critical roles in determining cellular identity in this pediatric cancer.
To better understand tumor biology, we focus on characterizing intra-tumor heterogeneity, not only for tumor cells but also in the surrounding tumor microenvironment. By studying the interactions between these compartments, we aim to unravel how they create an ecosystem that promotes tumor progression.
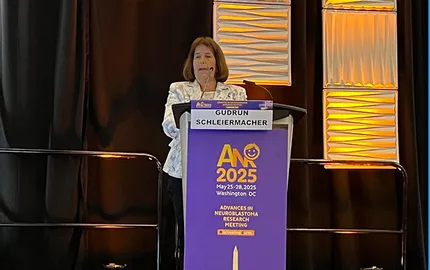
Our research integrates the analysis of cellular models, patient-derived xenografts (PDXs), and patient tumor samples, utilizing advanced omics approaches such as bulk and single-cell RNA-seq, ChIP-seq, and more. These studies leverage the cutting-edge technological platforms of Institut Curie and are complemented by functional assays. Patient material is obtained through collaboration with Dr. Gudrun Schleiermacher and clinicians of the SIREDO Center of Institut Curie.
Analysis of the tumor microenvironment in a cohort of 10 neuroblastoma patients (Figure 3) and the immunocompetent TH-MYCN transgenic mouse model revealed significant immunosuppressive features, including dysfunctional T lymphocytes and various immunosuppressive cells. Among these, a population of myeloid-derived suppressor cells (MDSCs)—also referred to as tumor-associated neutrophils—was identified. The immunosuppressive activity of these cells was confirmed through an ex vivo assay (Costa et al., Journal for ImmunoTherapy of Cancer, 2022).

Figure 3: Characterization of the tumor microenvironment in a cohort of 10 neuroblastoma patients by single-cell transcriptome analysis. NK: Natural Killer; TANs: Tumor-Associated Neutrophils; CAFs: Cancer-Associated Fibroblasts; cDC2: type-2 conventional dendritic cells. Publication: Costa et al, J Immunother Cancer, 2022.
In neuroblastoma patients, intratumoral T lymphocytes frequently express TIGIT and LAG3, that are molecules of the immune checkpoint family. In collaboration with Jan Molenaar’s team in the Netherlands, who similarly observed TIGIT expression in lymphocytes from neuroblastoma patients, it was demonstrated that the combined blockade of TIGIT and PD-L1 significantly reduced tumor growth in several preclinical neuroblastoma models (Wienke et al., Cancer Cell, 2024). These findings highlight the potential of developing anti-TIGIT antibodies as a novel immunotherapy approach for high-risk neuroblastoma.
Our team’s current research focuses on three major axes (Figure 4):
1. Intra-tumoral heterogeneity and cellular plasticity.
2. The tumor ecosystem and interactions between tumor cells and the microenvironment.
3. The role of MYCN and ALK oncogenes in the development of the sympathetic nervous system and tumor initiation.

Figure 4: The team's research focuses on unraveling the biology and mechanisms of oncogenesis in neuroblastoma, with the ultimate goal of developing more effective therapeutic strategies for children with high-risk forms of the disease.