- Home >
- News
Institut Curie News
Discover the latest news from Institut Curie.
Highlights
Search
Filter
Filter
Publication date
Fields
Search
200 result(s)



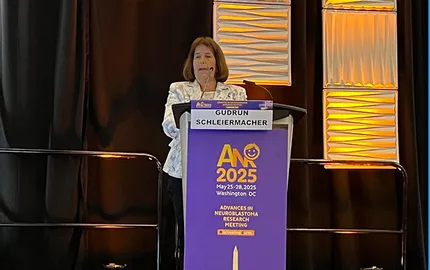
- Advances in Neuroblastoma Research Meeting
Pediatric cancers: how Institut Curie is advancing neuroblastoma research
26/05/2025